The Hidden Crisis: When Healthcare Systems Fail the Human Element
My sobering experience as a caregiver shattered every assumption I held about modern healthcare.
Roi Shternin
I have failed. I thought I understood healthcare from within, from all sides of it—as a patient first, but also as a clinician, researcher, manager, innovator, and caregiver. But apparently, my caregiving experience was sugarcoated. I had the sheer luck of landing in patient journeys that were far more privileged than others, particularly in certain oncological outpatient wards where I witnessed compassionate case managers, dedicated care coordinators, genuine empathy, and transparency paired with charitable organizations working to humanize the experience for both patients and healthcare professionals.
My previous encounter was with breast cancer care, and I was fortunate enough to design that very process in my role as advisor to that particular hospital. But this time—post-operation rehabilitation—was sobering and shocking in ways I never anticipated.
When Infrastructure Isn't Enough
I've witnessed plenty of understaffing and dysfunction in healthcare, but this experience was different. This wasn't the obvious lack of staffing, poor infrastructure, or overwhelmed staff that we've come to expect. This was a brand-new building with adequate professionals per shift and comprehensive systems designed to keep patients in the same ward except for imaging and surgical procedures. They had everything in-house: speech therapists, physiotherapy, occupational therapy, and even civil service staff to support the nurses.
Yet what took me by surprise was the stark reality that every single patient had a family member with them 24/7. I hadn't seen this in medical wards—only in pediatrics, where it's understandable. The reason became crystal clear: if you don't advocate for every single thing, the patient simply won't receive it. And I mean everything—diaper changes, assistance getting in and out of bed, eating, receiving medications, and being transported to treatments.
The Cultural Myth vs. Systemic Reality
Initially, I wondered if this was cultural—we are, after all, a close-knit society. But the truth was far more disturbing. This wasn't about culture; it was about burnout, the absence of patient-centered experience design, and overwhelmed staff who, despite their best intentions, had largely lost their capacity for empathy, compassion, and the clarity to see beyond the immediate clinical picture.
These healthcare professionals had stopped seeing broken people as they once were—parents, siblings, fellow human beings with rich histories and deep connections.
The Communication Catastrophe
I witnessed ignorance and communication breakdowns that even the world's most sophisticated IT systems couldn't fix. Departments operated in silos, refusing to communicate with one another. Caregivers weren't considered partners in the solution but rather targets for outsourcing nursing responsibilities—unpaid labor expected to fill systemic gaps.
The most heartbreaking part? I saw kind people who had lost their way, ground down by a system that demanded efficiency over humanity. But I also saw miraculous individuals who somehow managed to retain their empathy and compassion despite everything. These people should be studied, celebrated, and their approaches systematically implemented.
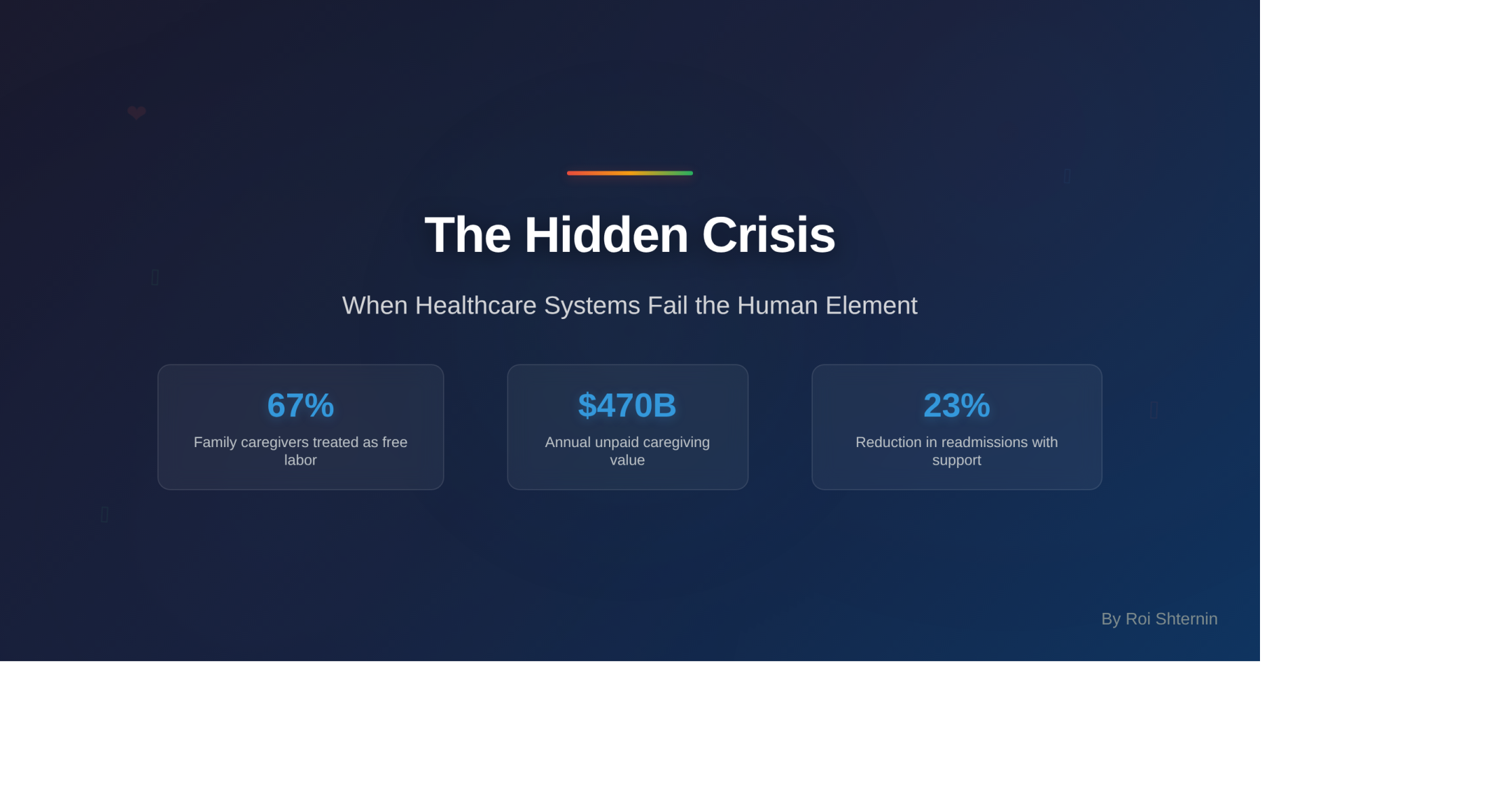
The Data Behind the Crisis
The statistics surrounding caregiver burden are staggering, yet largely ignored by healthcare administrators:
- 67% of family caregivers report that healthcare staff assume they will handle basic care tasks without proper training or support
- $470 billion annually—the economic value of unpaid family caregiving in the United States alone
- 40% higher burnout rates among healthcare professionals in systems that rely heavily on family caregiving to bridge gaps in care
These aren't just numbers. They represent millions of families thrust into roles they never trained for, expected to navigate complex medical systems while grieving, afraid, and exhausted.
Reframing the Solution: Caregivers as Partners, Not Plugs
The current model treats family caregivers as convenient gap-fillers rather than essential partners in healing. This isn't just morally bankrupt—it's strategically foolish. Research consistently shows that when family caregivers are properly integrated, trained, and supported, patient outcomes improve dramatically:
- 23% reduction in hospital readmissions when families receive structured support
- 35% improvement in medication adherence with proper caregiver education
- Significant decreases in medical errors when communication includes family members as informed partners
The Empathy Paradox
Here's what healthcare leaders refuse to acknowledge: the professionals who maintain their empathy aren't superhuman. They work within systems that actively support emotional sustainability. They have manageable caseloads, adequate resources, and leadership that recognizes emotional labor as essential work, not weakness.
The burned-out professionals aren't failures—they're canaries in the coal mine, warning us about toxic systems that consume human compassion as readily as they consume budgets.
A Call to Revolutionary Change
We stand at a crossroads. We can continue accepting healthcare systems that treat caregivers as free labor and professionals as replaceable cogs, or we can demand fundamental transformation.
For Healthcare Leaders: Transform your perspective on family caregivers from burden to asset. Invest in comprehensive caregiver support programs, not as charity, but as strategic imperatives that improve outcomes and reduce costs.
For Policymakers: Recognize caregiving as essential infrastructure. Just as we invest in roads and bridges, we must invest in the human connections that make healing possible.
For Fellow Caregivers: Your advocacy isn't just necessary—it's revolutionary. Every time you demand better communication, insist on inclusion in care planning, or refuse to accept inadequate support, you're fighting for systematic change that will benefit countless others.
The Healthcare We Deserve
Imagine healthcare systems where family caregivers receive training, support, and recognition as essential partners. Where professionals work in environments that sustain rather than drain their capacity for compassion. Where patients receive care that honors their humanity, not just their diagnosis.
This isn't utopian thinking—it's evidence-based transformation. Organizations implementing comprehensive caregiver support programs report improved staff satisfaction, better patient outcomes, and reduced costs.
We're not asking for charity. We're demanding recognition of our inherent value and the systematic changes necessary to honor it. The future of healthcare isn't about managing scarcity—it's about recognizing abundance in human connection and designing systems worthy of our collective care.
The question isn't whether we can afford to make these changes. The question is whether we can afford not to.
Want to collaborate in creating a better healthcare? Reach out to me at talks@roishternin.com