Why Case Management is Our Only Path Forward
The Architecture of Care: Why Case Management is Our Only Path Forward
By Roi Shternin
We live in the liminal spaces between sickness and wellness, between the body we remember and the body we inhabit. Chronic illness is not a destination but a country with shifting borders, where the landscape changes without warning and the maps we carried into this territory become obsolete with each passing season.
I have learned to speak the language of appointments, the dialect of symptoms carefully catalogued and presented like evidence in a courtroom where the jury is always deliberating. But beneath this careful choreography of medical compliance lies a deeper truth: we are drowning in the fragments of a healthcare system that sees us as collections of parts rather than whole beings navigating an impossible geography.
The Masquerade of Functionality
Each morning, we don the armor of normalcy. The makeup that conceals the exhaustion. The practiced smile that suggests we are managing well. The careful calibration of energy that allows us to appear functional in a world designed for bodies that bend without breaking. This is the masquerade we perfect—not out of vanity, but out of survival.
The current healthcare paradigm asks us to be our own translators, our own advocates, our own cartographers of pain. We learn to speak multiple medical languages, to carry files and histories like sacred texts, to remember which doctor knows which part of our story. We become archeologists of our own suffering, excavating symptoms and side effects, medication interactions and appointment conflicts, insurance denials and prior authorizations.
But what happens when the translator becomes too tired to translate? When the advocate loses their voice? When the cartographer can no longer read their own map?
The weight of this performance is crushing. We smile through the fatigue that settles in our bones like winter frost. We nod understanding when specialists speak past us rather than to us. We carry the burden of proof that our suffering is legitimate, our needs real, our humanity worthy of recognition. The mask becomes so familiar that sometimes we forget what our face looks like beneath it.
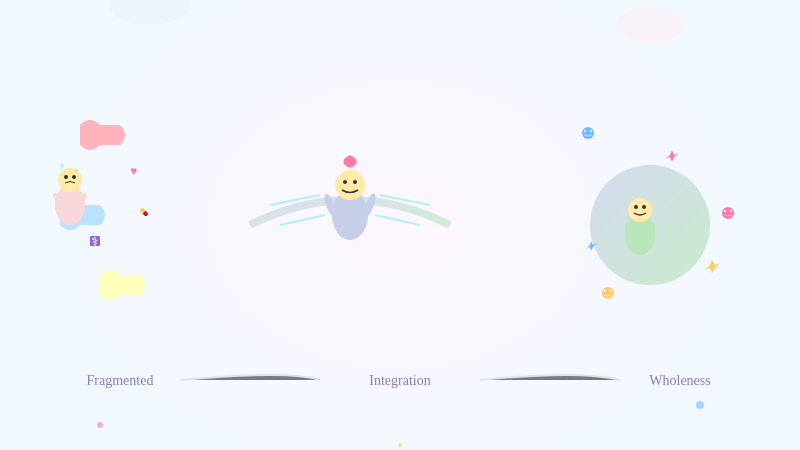
The Fragmentation of Being
In the absence of coordinated care, we splinter. The cardiologist knows our heart but not our sleep patterns. The rheumatologist understands our joints but not our mental health. The psychiatrist medicates our mind but cannot see how it connects to the inflammation coursing through our bloodstream. We become living case studies in medical specialization—a heart here, joints there, a mind floating somewhere in between.
This fragmentation mirrors the internal fracture that chronic illness creates. We learn to compartmentalize not just our symptoms but our very selves. The person who suffers becomes separate from the person who functions. The body in pain becomes disconnected from the spirit that endures. We master the art of living in pieces because our care exists in pieces.
Yet what if there was another way? What if someone could hold all the fragments of our experience and weave them into a coherent narrative of care?
The Revolutionary Act of Wholeness
Case management is not merely administrative coordination—it is a revolutionary act of seeing the person within the patient. It is the recognition that chronic illness is not a medical problem with social implications, but a human experience that requires medical intervention within a complex web of needs, relationships, and realities.
A skilled case manager becomes the keeper of the whole story. They understand that the missed appointment might be about transportation, not non-compliance. That the medication adherence issues might stem from financial stress, not forgetfulness. That the frequent emergency room visits might signal not drug-seeking behavior, but a failure of preventive care coordination.
They become the translators we desperately need—not just between medical jargon and human language, but between the fragmented pieces of our care team. They are the advocates who fight battles we are too exhausted to fight, the navigators who can read the maps when our hands shake too much to hold them steady.
The Anatomy of the Perfect Case Manager
In my years of navigating the labyrinth of chronic care, I have encountered case managers who barely qualify as administrators, and others who transform lives through their presence. The difference lies not in credentials alone, but in a particular alchemy of skills, wisdom, and humanity.
The perfect case manager is part detective, part diplomat, part warrior. They possess the clinical knowledge to understand complex medical conditions while maintaining the emotional intelligence to recognize when a patient's resistance to treatment stems from trauma, fear, or despair rather than defiance. They are bilingual in both medical terminology and human suffering.
They must be comfortable with ambiguity, because chronic illness rarely follows textbook patterns. They need the patience of a teacher, the persistence of an investigator, and the compassion of a friend who has walked through darkness and emerged with lanterns for others. Most importantly, they must understand that their role is not to fix us, but to help us navigate toward our own version of wholeness.
The perfect case manager sees patterns where others see chaos. They notice when a patient's missed appointments correlate with their spouse's work schedule, or when medication non-adherence follows the monthly rhythm of financial strain. They understand that healthcare happens not just in clinical settings, but in the mundane moments of daily life—the kitchen where medications are organized, the bedroom where sleep is either found or lost, the workplace where accommodations mean the difference between dignity and desperation.
They are advocates who speak truth to power, whether that power resides in insurance companies, healthcare systems, or physicians who have forgotten that behind every chart lies a human story. They fight for coverage denials to be overturned, for appointments to be scheduled when patients can actually attend them, for treatment plans that acknowledge the reality of limited energy and resources.
Technology as Translator, Not Master
Technology, when thoughtfully implemented, can amplify the case manager's ability to hold and weave together the complex threads of our care. But technology alone is not the answer—it is simply a tool that must be wielded with wisdom and compassion.
Imagine a system that learns the rhythm of your illness—when your energy typically ebbs and flows, when your symptoms tend to flare, when you are most likely to need intervention before crisis strikes. Not to replace human judgment, but to provide the case manager with insights that might otherwise remain invisible in the chaos of managing multiple complex cases.
Electronic health records could evolve beyond repositories of clinical data to become living documents that capture the full context of a person's experience. Not just vital signs and lab results, but social determinants, personal goals, family dynamics, and the subtle patterns that only emerge when someone is paying attention to the whole person over time.
Artificial intelligence could serve as a pattern recognition assistant, identifying potential drug interactions not just between medications, but between medications and life circumstances. It could flag when a patient's digital footprint suggests depression, isolation, or non-adherence before these issues manifest as medical crises.
But technology must never replace the irreplaceable human capacity for empathy, intuition, and the kind of presence that makes someone feel seen and heard. The perfect technological tool is invisible—it enhances the case manager's ability to be fully present with their patients rather than distracted by administrative burden.
The Infrastructure of Compassion
Creating effective case management requires more than hiring compassionate individuals and hoping for the best. It demands a fundamental restructuring of how we conceive of healthcare delivery, compensation models, and success metrics.
Case managers need time—something the current healthcare system treats as a luxury rather than a necessity. They need manageable caseloads that allow them to actually know their patients rather than simply manage their files. They need access to resources that extend beyond medical interventions to include social services, mental health support, transportation assistance, and the myriad other supports that make adherence to treatment possible.
They need authority to make decisions and solve problems in real-time rather than being constrained by bureaucratic layers that turn urgent needs into administrative delays. They need compensation structures that reward relationship-building and prevention rather than crisis intervention and volume metrics.
Most importantly, they need institutional support that recognizes case management as skilled professional work rather than administrative overhead. This means training that goes beyond clinical knowledge to include communication skills, cultural competency, trauma-informed care, and the complex art of navigating healthcare systems on behalf of vulnerable populations.
The Economics of Seeing Whole
The resistance to comprehensive case management often centers on cost, as if caring for human beings in their full complexity is somehow a luxury rather than a necessity. But what is the true cost of our current system? What price do we place on the emergency room visits that could have been prevented, the hospitalizations that result from medication interactions, the lost productivity when people cannot access coordinated care?
More fundamentally, what is the cost of asking human beings to fragment themselves to fit into a system that refuses to see them whole?
Case management is not an additional expense—it is an investment in the radical idea that people with chronic illnesses deserve care that acknowledges their full humanity. It is the recognition that health exists not in isolation but in relationship, not in specialization but in integration.
The economic argument for case management becomes compelling when we consider the downstream effects of coordination: fewer emergency interventions, better medication adherence, improved health outcomes, reduced family caregiver burden, and the preservation of human dignity that allows people to remain productive members of their communities.
The Path We Must Take
There is no other way forward. The current system is not merely inefficient—it is unsustainable and inhumane. As the population ages and chronic illness becomes increasingly prevalent, we cannot continue to ask individuals to serve as their own case managers while simultaneously denying them the tools and support to do so effectively.
But transformation requires more than policy changes and funding shifts. It demands a fundamental reimagining of what healthcare means, who it serves, and how success is measured. It requires recognizing that health is not simply the absence of disease, but the presence of conditions that allow human beings to flourish within the constraints of their circumstances.
We who live in the country of chronic illness are not asking for special treatment. We are asking to be seen whole, to be cared for completely, to have our full humanity acknowledged in our pursuit of health and healing. We are asking for case management that recognizes that our conditions are not problems to be solved but realities to be navigated with skill, compassion, and unwavering commitment to our dignity.
The technology exists. The knowledge exists. The compassionate professionals exist. What we need now is the collective will to create systems worthy of the humans they serve. Case management is not a luxury for the privileged few but a fundamental right for anyone navigating the complex terrain of chronic illness.
The path forward is clear. The only question is whether we have the courage to take it, and the wisdom to understand that in caring for the most vulnerable among us, we create a healthcare system worthy of us all.
In the spaces between appointments, in the silence after diagnosis, in the moments when hope feels like a luxury we cannot afford, we wait. We wait for a system that sees us whole, that holds our complexity with competence and compassion, that recognizes that our healing is not separate from our humanity but inseparable from it.
The architecture of care we envision is not just about case management—it is about the radical act of building a world where suffering is met with wisdom, where complexity is embraced rather than simplified, where every person navigating the territory of chronic illness has a skilled guide who knows both the terrain and the destination: not the impossible return to who we were before, but the precious discovery of who we might become in the fullness of our experience.
This is our call. This is our hope. This is the only way forward.
I'm a health revolutionary trying to make life easier for both patients and the ones caring for them, join my revolution at Chronically.health